Your Custom Text Here
Can CranioSacral Therapy Help Multiple Sclerosis?
Last fall I set out to do a case study on a friend who has advanced Multiple Sclerosis (MS). His health took a more steep dip in 2020 to the point where he found day-to-day activities like walking and showering more challenging. CranioSacral Therapy (CST) has helped me immensely in healing from severe head trauma as a child, and I’ve seen it do wonders for my clients with histories of physical as well as emotional trauma. I wanted to see if it would help my friend and his symptoms related to MS.
Multiple Sclerosis is an autoimmune condition without a known cure where the immune system attacks the myelin sheath of the body’s nerves. Common symptoms include chronic pain, difficulty moving, vision and speech issues as well as anxiety/depression. CranioSacral Therapy (CST) is a gentle, hands-on technique that seeks to improve the function of the Central Nervous System and other body systems that relate to it, including the Immune System. If the Sympathetic Nervous System remains activated for long periods of time (as it would with chronic stress and/or trauma), it also affects the ability of the Immune System to do its job properly. Side note that this is why so many folks with autoimmune conditions also have trauma/PTSD backgrounds, or that a stressful event(s) triggers a condition. So, can and did CST help my friend and his pain?
A little background on my study subject: 63 year-old-male, diagnosed with MS in 2010 in tandem with optical neuritis and vertigo. We did the basic, 10 Step CST protocol, administered 8 weeks in a row, with steps in the same order over the course of a 60-minute session. I used the McGill Pain Questionnaire, a self-reported survey, which delineates different types of pain and ascribes a number for an individual’s pain level—that way we could quantify whether or not the work helped him. Maximum possible score is 78; the higher the number, the more pain the individual is experiencing.
When we began the study, he reported a pain level of 62 out of 78 and most acutely felt pain in the lower back and hip regions with spasticity. He also felt a concentration of pain in how his mental health was impacted, experiencing fear as well as intense to unbearable pain (these were boxes on the questionnaire).
After 8 weeks, he reported a 60% improvement in pain (37 of 78) with less tension and numbness. How the pain affected his mental health was the most significant area of improvement. Initially, he selected adjectives such as agonizing and dreadful (higher on the pain scale) whereas in the second evaluation he only selected nagging (the lowest). In general, he felt more calm, less anxious and was experiencing better quality of rest. Another note here, we did this study in the 8 weeks preceding the election. So, the fact that he had a greater sense of ease is even more telling of the work and how it can help you or someone you know.
A lot of massage therapists and chiropractors are trained in this technique. If you have a history of anything I mentioned: PTSD, trauma, concussion and/or autoimmune issues, try a few sessions of CranioSacral to see if it helps your mental and physical health. It’s super relaxing—promise you’ll have a good sleep that night.
The Body Keeps Score
Did you know that if you (or someone you know) have suffered through abuse, a traumatic event or upbringing that the brain actually shifted as you (they) attempted to process the pain? This book has rocked my world the past couple of weeks in learning how amazing the body is and how healing from trauma is a layered process.
What is trauma?
In short, something that was stressful in which you felt alone. Obvious examples here include abuse, natural disaster, loss, terrorism and war. In looking at the behavioral patterns that can arise from trauma, I can't help but think most of us could cite some form of traumatic event(s)/relationship(s) in our lives.
How does the brain shift?
Trauma can actually change the brain's alert system and responding hormones in addition to leaving a mark on the brain similar to a stroke. The author, Bessel Van der Kolk, conducted a study where he showed participants images to trigger their trauma while monitoring their brain hemispheres. When participants were exposed to traumatic images, the right side of the brain that impacts how we perceive the world around us was activated, while the left, organizational side deactivated. The brain itself is in response mode to the trigger without real context of time or place. Moreover, the brain's response to trauma is pre-verbal so this explains why recounting what happened in a logical or coherent manner may be difficult or garbled.
While one may consciously choose not to respond to a trauma trigger, the body systems are still reacting, including hormones, which don't return back to normal levels after being in fight or flight or freeze mode. Because of this there is an internal disconnect so one may suffer from addiction or self-mutilation as well as illness, adrenal fatigue, fibromyalgia/chronic fatigue, poor sleep, memory issues, autoimmune disorders and irritability. (If you're super geeky about this stuff, as I am, he spends a good 10 pages going into brain chemistry specifics...but does so in a very approachable way for the brain science novice.)
What are some symptoms of trauma?
Hyper-vigilance-Because of the brain shift, one can be in a perpetual state of hyper-vigilance. This goes back to the perception lens--the brain is constantly surveying for a potential threat. This also means that one may project past traumas onto current life events.
Social isolation-Not wanting to engage with others because this could set off a trigger, so it's better to avoid interaction. On the flip side, fraternizing with those who have suffered the same trauma may feel safe (e.g. other veterans) yet this can also be limiting over time as one's identity shifts.
Loss of identity-You may more commonly know this as survivor's guilt as well as confusion if the person who abused you was supposed to be your caretaker/loved one.
Emotionally numb-A way to deal with the trauma is to disassociate from one's body and feelings, leaving one devoid of feeling.
Loss of imagination-If raised in an unsafe environment, all of the body's systems are in self-preservation (hyper-vigilance) mode so there's no room for imagination or exploration.
Risk-taking-The body releases endorphins which are like morphine, so one can become addicted to risks or even find pleasure in pain. The body seeks this out to overcome anxiety.
How does one heal?
The author suggests 3 approaches to be used in tandem as needed.
- Top down with talk therapy, specifically EMDR, Internal Family Systems and Neurofeedback. If you're in Austin, there's a great clinic that uses these approaches. Find out more about them here.
- Medications that will turn off the body's alarm systems.
- Bottom up through the physical so that the body can experience something other than helplessness and rage which gets held in the viscera (i.e. having a broken heart, stomach in knots). He suggests this in particular for those who suffer from musculo-skeletal pains that may have an emotional root. Since that is my bag and this is my blog, I'm going to spend a bit more time on this and his suggestions.
Heal trauma with mindfulness.
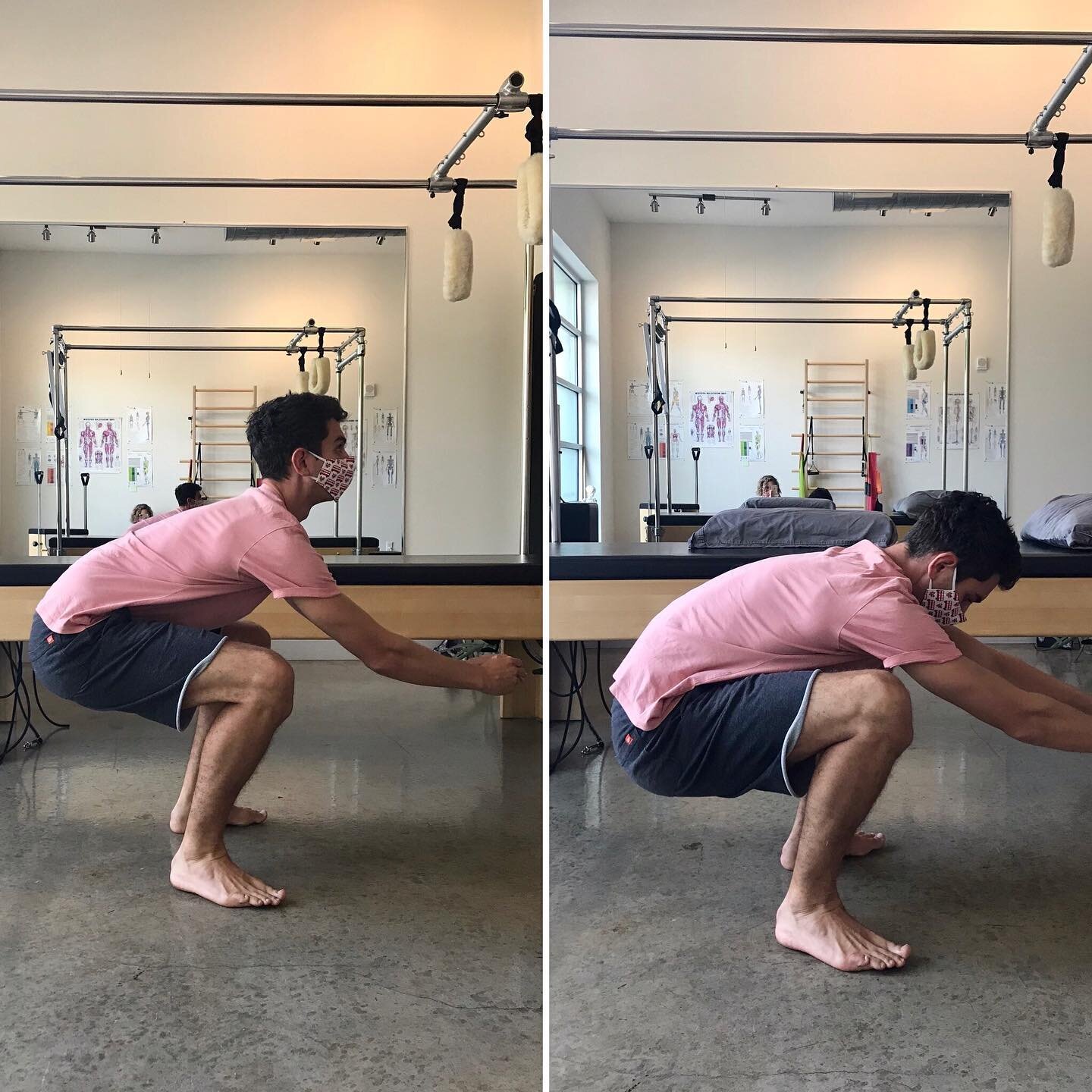
Ki Hara Active Stretching for mindfulness and flexibility.
The first step in releasing the past is reconnecting with and establishing ownership of the body to feel, find peace and focus so that when things trigger the past, one can maintain internal calm. When we can connect with how we feel, we can begin to change perspective. If we can't feel, we are incapable of figuring out what our body needs and how we can best take care of it. By being present in our bodies, it is safe to revisit the past without being overwhelmed by it. We can start to have words for things we may have hidden from ourselves and reintegrate the pieces of ourselves that we've lost along the way. A way of coping with trauma is disassociating from our bodies, so mindfulness and breath work reaffirm who we are as a whole being.
The author recommends yoga as an avenue to mindfully connect with the body. A former client of his specifically cited that Pilates helped her heal from a traumatic event to her pelvis. I love both of these modalities, yet I don't think I learned to be deeply connected to my own body until I encountered Ki Hara Resistance Stretching (aka yoga on steroids). It has been amazing for helping myself and my clients reconnect with areas of the body that have been forgotten and then integrating them to the whole. It's particularly effective because when I'm working with a client, it becomes a partner effort to rediscovery. In other words, it's not someone alone in their own stretching practice (though this is another component for establishing ownership of one's body). I can be an objective pair of eyes for how your body is moving when there could be a more efficient way. If you haven't connected to a part of your body in a long time, how are you even supposed to know it's there?
I found this book to be incredibly insightful both for my own understanding of some areas I need to work on and to have more compassion for others who have are trying their best to heal. If you're one who is better with video over books, here's an interview with the author with some similar themes.
How strong are your respiratory muscles?
Take a moment and start counting the duration of your inhalation and exhalation. Does the pace at which you're breathing feel like your normal? Is it easier to inhale or exhale? Where do you find the breath entering and exiting? Does it most easily move in and out of your belly or your upper chest? Do your lower ribs move when you exhale? I find that most people don't move their lower ribs in the respiratory cycle, which means they're missing out on a full breath. This can go on for years and impacts pretty much every other system in your body, including your digestive and nervous systems.
How does the breath cycle work?
The diaphragm acts as a plunger system, pulling air into our bodies and filling our lungs (fun fact: the lungs are kind of like origami-folded tissue that unfolded are the size of a tennis court). The diaphragm is a muscle, so it has a full range of motion like any other muscle, yet most of us only 'exercise' it in a very short range. We shallowly breathe due to stress and holding a posture that we think is 'good', more on that in a moment. If you consider how the diaphragm typically works in this short cycle, it would be like doing thousands of tiny bicep curls all day long--sounds kind of funny when you think about it that way, right? The diaphragm is the main breathing muscle, yet there are several other secondary muscles that help out. One of my favorite groups is the intercostals. These muscles glide in beteeen each rib and help to expand and contract our rib cage. They are, however, weak for most folks.
How do the intercostals weaken and why should I take ever loving care of them?
As previously mentioned, most of us breathe shallowly as a stress-holding pattern. For some, this means weak and tight intercostals, so it's hard to inhale and expand them. For others, they're weak and puffed out (barrel-chested) and it's harder to exhale. In the latter case, I find that people assume this posture thinking they have good and confident posture--yet you can't breathe. Another way this pattern can occur is from sucking the stomach in or wearing restrictive clothing. Try sucking your stomach in right now and you'll feel your rib cage puff. Either way, we want these guys to be able to expand and contract fully, just like our biceps.
Strong intercostals and respiratory muscles help massage your stomach as you breathe, enabling your digestive system to do its thing. They also help to keep your nervous system at ease and not in fight-or-flight mode. As an added bonus, you're strethening your core muscles, which will give you organic, proper posture. If you're active, tapping into a full breath cycle, including the plunger power of your diaphragm, will take your athletic abilities to the next level.
How do I strengthen my respiratory muscles?
To start, be more conscious of your breath. I love the count breath. Try to equal out your inhalation and exhalation and then gradually add another count. Say you start at a 4 count, can you gradually reach your way to an 8? As you continue to add time, focus on squeezing the air out of your rib cage during the exhalation, contracting your intercostals.
You can also try these exercises over a towel, ball, pillow or foam roller.
I integrate breath work into my sessions with clients so that you can grow these muscles, bettering your digestive and nervous systems, while improving your posture and core. In finding your breath, you find your power!
Why is my body tight?
Full body, active Ki Hara stretching! Soooo yummy!
This is a question I'm often asked and believe that we have to look at more than just range-of-motion or trigger points for a good explanation. Some clients immediately tell me that their body is tight because it runs in their family, like they have an inflexiblity gene and traditional stretching just doesn't work for them. I see body tightness that runs in families as a cultural way that the family deals with stress and how we then handle stress as adults. Are things shoved under the rug or not acknowledged? Or, are things discussed and worked through together? Do you feel overwhelmed and overburdened by responsibility? Or, are you able to shift your perspective and carve out some self-care time?
The nervous system automatically charges up to help when we're stressed (sympathetic nervous system). One result when it kicks in is that the muscles tighten to prepare for action--we can see this in animals. When they perceive a threat, the breath cycle shortens, their whole body tightens and is ready to pounce. When we, as humans, hold in this way everyday, it leads to chronic body tightness and fatigue.
To offset this stress from a movement perspective, we most often think exercise. Yet, how many of us hold our breath when we try to burn off some steam? Muscles can't relax if they're being starved of oxygen. As someone who is also prone to this, I've started doing some diaphragm releases to connect with my breath before I intentionally move. This is my favorite diaphragm release to do pre-workout.
Ki Hara active stretching unwinds tension from the body, creating space for more breath. Clients always stand up at the end of a session saying they feel more alive, relaxed and have more blood flowing through their body. We target the areas you personally hold tension and dynamically release muscle tension there. Full body stretching like in the photo above, allows for the body to have a feeling of flow over bracing. To learn more, click here.